Scott Wittet (left to right), PATH and Cervical Cancer Action; Joanna Cain, International Federation of Gynecology and Obstetrics; Ambassador Sally Cowal, American Cancer Society; David Fleming, PATH; Catherine Guinard, Cancer Research UK; Jose Jeronimo, PATH and Debbie Saslow, American Cancer Society
The global burden of cervical cancer is high, and it is inequitable between and within countries. An estimated 266,000 women die from the disease every year, with 85% of deaths in developing countries. Twenty-five percent occur in India alone. In many countries, cervical cancer is the number one cancer killer of women and it now kills more women than childbirth in many regions (1). Nearly all of these deaths are preventable by scaling existing interventions to reach as many individuals as possible.
The World Health Organization (WHO) estimates that by 2030, the total number of cervical cancer deaths is expected to rise to 443,000 globally, more than double the anticipated number of deaths from pregnancy-related complications (estimated to be 200,000) (2). The global cost of cervical cancer was estimated to be US$ 2.7 billion per year in 2010 and is expected to rise to US$ 4.7 billion by 2030 (3).
Cervical cancer kills at a comparatively young age, so families lose their mothers and grandmothers, they suffer economic loss, and the lives of their children are put in jeopardy. The women at highest risk for cervical cancer are also those who may currently be benefiting from maternal health and HIV programmes in low- and lower-middle-income countries. Women who are HIV positive are at increased risk of cervical cancer, and platforms for HIV/AIDS treatment could be used for cervical cancer screening programmes, so organizations that deal primarily with prevention of HIV/AIDS — such as the Joint United Nations Programme on HIV/AIDS (UNAIDS) — now also are prioritizing cervical cancer prevention. They feel that it does not make sense to save a woman from AIDS only to lose her a decade later to another preventable disease.
Virtually all cervical cancer is caused by oncogenic types of the human papillomavirus (HPV). While most women (and men) are infected with the HPV types responsible for cervical cancer within a few years of becoming sexually active, only a small percentage of women become chronic carriers of the virus and a minority of them develop cervical precancer and cancer (4). Strategies for prevention of cervical cancer focus on blocking infection through HPV vaccination (primary prevention) and detection and treatment of precancer to avoid development of cervical cancer (secondary prevention). Treatment of advanced cervical cancer is difficult and costly, and the skills and equipment necessary for treatment are in short supply in low-resource countries, so prevention is paramount. This article focuses on cervical cancer prevention, not the treatment of advanced disease.
Oncogenic types of HPV also cause other cancers, including penile cancer, anal cancer, vaginal cancer and head and neck cancers. Some non-oncogenic types of HPV cause genital warts, a very common sexually transmitted disease.
We have effective and affordable solutions at hand
Compared to other cancers, cervical cancer is relatively simple and inexpensive to prevent with current technologies. Resource-rich countries have radically reduced cervical cancer rates over the past 50 years, primarily due to the widespread and repeated use of the Pap smear (cytology) for screening (5). But cytology has limitations due to geography and availability, even in wealthy countries, and has not proven sustainable or scalable in low-resource areas (6). However, two new and complementary prevention options — HPV vaccination for young adolescent girls, combined with low-cost screening and preventive treatment of adult women (treatment of cervical precancer) — could reduce cervical cancer deaths in lower-resource countries to the very low levels currently observed in Australia, Europe, the United States and other countries.
HPV vaccination
Vaccines against HPV are powerful, lifesaving technologies. Presently two HPV vaccines are widely available and have been licensed as safe and effective in over 120 countries. The vaccines are effective at preventing pre-cancerous cervical lesions when given to young adolescent girls prior to infection with HPV (before sexual initiation) (5). They are expected to prevent the majority of cervical cancer cases, based on the two oncogenic HPV types (16 and 18) associated with about 70% of cervical cancers (7, 8). Both vaccines also have excellent safety records. Among the millions of doses given worldwide, very few serious side effects have been related to HPV vaccination, especially in the young adolescent age group (9, 10). To date, WHO reports no deaths from HPV vaccination (5). A 9-valent vaccine (with five additional oncogenic HPV types) was approved in late 2014 but is not yet widely available; it is expected to prevent about 90% of cervical cancers (11).
Young adolescent girls and boys both can benefit from HPV vaccination when protecting both sexes is affordable. Vaccinated men would be less likely to infect women, and the boys would be protected from other cancers caused by certain HPV types. However, when funding is limited, and when focusing on the prevention of the major killer, cervical cancer, the WHO, Cervical Cancer Action (CCA), and many other organizations recommend vaccinating as many young adolescent girls as possible as the most cost-effective HPV immunization strategy (5, 12).
Acceptance of HPV vaccination has been high in low-resource countries, in part because in settings where most patients are not sequestered in hospital cancer wards, it is not unusual for people to recognize — and be concerned about — the symptoms of cervical cancer. In those parts of the world we generally have not seen parental pushback against vaccination due to concerns about sexual disinhibition (though that sometimes occurs in the United States and Europe). Successful programmes have chosen not to over-emphasize that the vaccine prevents a sexually transmitted infection; instead the focus of messaging is on cancer prevention.
Many countries offer HPV vaccine to adolescents of the appropriate age through public-sector vaccination programmes. Use of HPV vaccine in low- and lower-middle-income countries has progressed rapidly since 2013 when GAVI, the Vaccine Alliance began offering the vaccine at a subsidized rate to the poorest countries in the world.
Cervical precancer screening and preventive treatment
The hundreds of millions of women who were already infected before the vaccines became available, and vaccinated girls who will become infected with HPV types not prevented by current vaccine formulations, require secondary prevention. Fortunately, new technologies for screening and preventive treatment (using cryotherapy, thermal coagulation, or other methods) can protect substantial numbers of those women affordably and effectively without the need for expensive and technically challenging cytological testing (5). Developing basic screening and treatment services for women using these proven new tools will save lives within a few years and will create a platform for introduction of even more effective screening tests currently in development (13). Lower-cost alternatives to Pap smears have proven effective in low-resource settings — these include visual inspection with acetic acid (VIA) (which allows providers to see pre-cancerous lesions during a pelvic examination, with sensitivity as high or higher than cytology) and HPV testing (new molecular tests for HPV DNA or RNA or for markers of precancer or cancer) (5, 14). Modeling suggests that screening (and treating) a woman just once in her lifetime can result in significant reductions in cervical cancer risk (15).
VIA-based programmes are currently being implemented in multiple low-resource countries and regions, though most are not yet large scale. However, Bangladesh, El Salvador, Ghana, Guatemala, Indonesia, Kenya, Malawi, Tanzania, the Philippines, Uganda and Zambia, among others, are developing population-based screening programmes using VIA (12).
HPV testing holds particular promise as a screening method, both because of its high sensitivity and because it can be done through self-collection of vaginal samples if the availability of trained providers, cultural sensitivities, or geography are barriers to screening using cervical samples (trading slightly lower sensitivity for vastly increased potential for deployment at population levels). Vaginal sampling makes testing more attractive and convenient for many women and could allow programmes to scale up screening in a cost-effective manner (15, 16).
It is crucial to note that HPV testing does not obviate the need for VIA (or another way to visualize the cervix) because visualization is necessary to determine what type of treatment is appropriate for HPV-positive women. Widespread use of HPV testing will reduce the number of VIA procedures necessary since only HPV-positive women would be referred for examination, thereby reducing the burden on health systems. The cost of HPV testing is decreasing and tests appropriate for field use are becoming increasingly available.
For these reasons, for areas initiating screening, CCA recommends establishing VIA-based programmes as soon as possible to save lives now and to create a platform into which HPV testing (or other, future molecular tests) can be introduced as soon as feasible.
Cryotherapy (freezing tissue) is a simple and relatively low-cost preventive treatment and is appropriate for the majority of precancer cases (5). Alternatively, thermal coagulation (also called cold coagulation) may be used and may avoid some of the programmatic challenges inherent in cryotherapy-based approaches (17). Some precancer cases require other procedures, such as the loop electrosurgical excision procedure (LEEP).
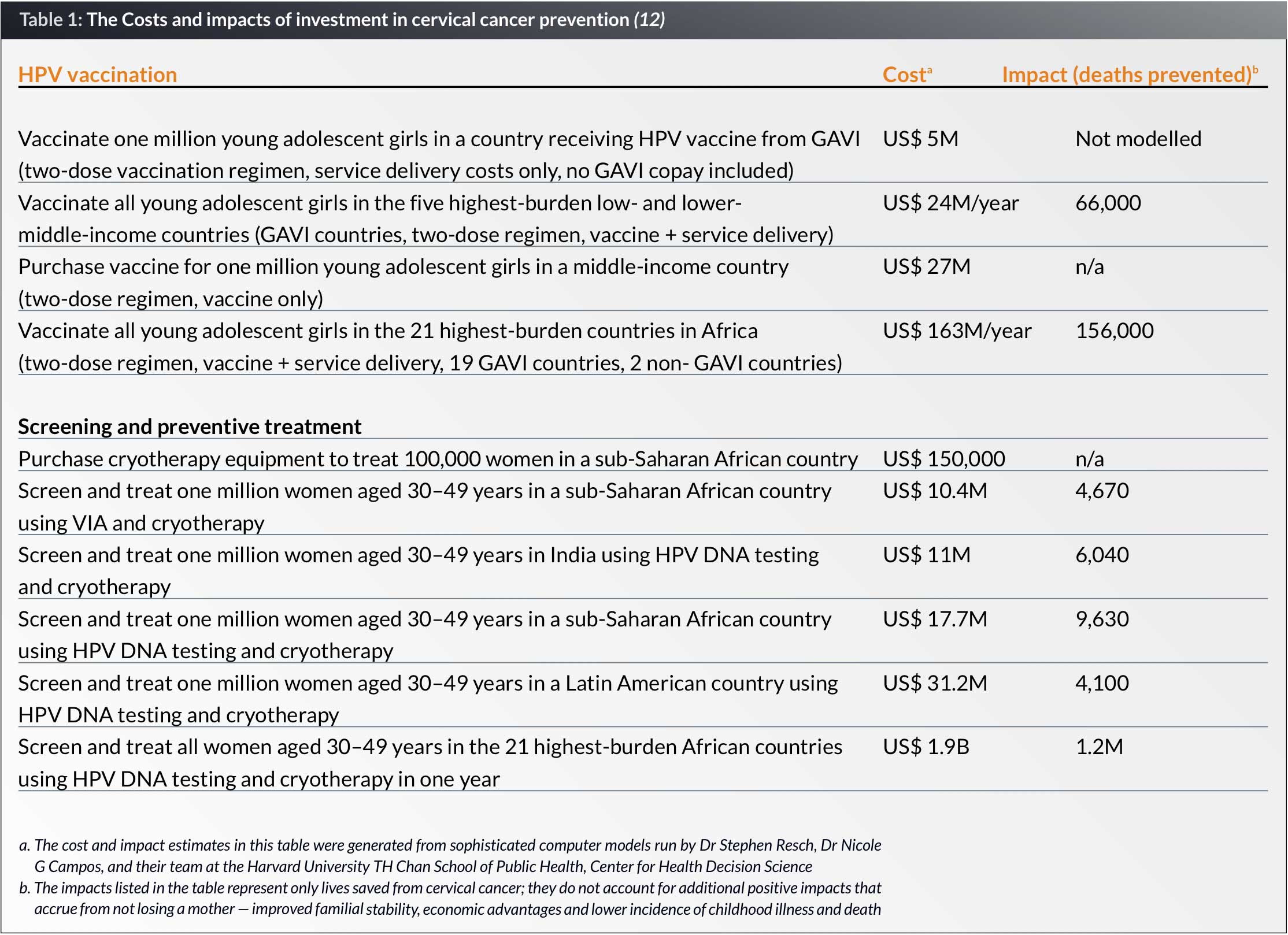
International and national investments are needed to scale up prevention
Cervical cancer prevention is a wise investment and WHO calls cervical cancer screening and preventive treatment a “best buy” in public health (18). A recent costing study estimates that US$ 3.5 billion will be necessary over the next decade to vaccinate all 10-year-old girls and provide screening and preventive treatment using VIA or HPV testing for all 30- to 49-year-old women at least once in their lifetimes (19). The same modeling exercise calculated the costs and impacts of sample interventions in selected geographic areas (see Table 1).
Programmes in Africa, Asia and Latin America have shown that HPV vaccination, VIA- or HPV-test-based screening, and preventive treatment can work in low-resource settings and have the potential for significant and lasting impact (5). CCA tracks the expansion of these programmes worldwide on its website (20). As of December 2015, 44 low- and lower-middle-income countries had introduced HPV vaccine and 53 had introduced new screening and preventive treatment modalities on a pilot or national basis. However, because many of these programmes are relatively small-scale pilots, the vast majority of women worldwide do not yet have access to screening and preventive treatment, and many more girls must be vaccinated.
A new initiative to mobilize resources for cervical cancer prevention
CCA, a global coalition to stop cervical cancer, along with an expanding roster of partners, seeks to accelerate the introduction and scale-up of both HPV vaccination and pre-cancer screening and preventive treatment where they are needed most. On 3 to 4 November 2015, CCA hosted a high-level conference in London called “Investing in Cervical Cancer Prevention 2015–2020”. The conference brought together key partners to take stock of recent global progress in cervical cancer prevention, spur expanded action and investment, and establish a consensus vision for what is required to meet our global goals and safeguard our commitments to the health of women and adolescent girls. The conference was attended by 75 individuals representing 44 international agencies, including the CCA Governing Council partners, The Global Fund to Fight AIDS, Tuberculosis and Malaria; UNAIDS; the Bill & Melinda Gates Foundation; Rotary International; the UK Department for International Development; the United Nations Children’s Fund (UNICEF); the United Nations Population Fund (UNFPA); and WHO. Representatives hailed from Argentina, the Democratic Republic of the Congo, Ghana, Uganda, the United States, Europe, Zambia and Zimbabwe (21).
At the conference, CCA and its partners launched Taking Cervical Cancer Prevention to Scale: Protecting All Women and Girls, a five-year global initiative to tackle the growing burden of cervical cancer in low- and lower-middle-income countries (22). The Initiative aims to ensure that all young adolescent girls have access to the HPV vaccine and that every woman can be screened at least once between the ages of 30 and 49 — and that she has access to precancer treatment when necessary.
The Initiative has four goals:
- Scale up prevention services for all women and girls. Build political commitment for developing appropriate policies and integrating vaccination and screening/ preventive treatment into school health, women’s health and HIV/AIDS prevention and treatment programmes. For partners currently operating limited prevention programmes, seek to cover all girls and women.
- Expand the stakeholder base globally and in countries. Strengthen and expand national- and global-level commitments and investments in cervical cancer prevention, and support collaboration for more effective implementation.
- Encourage innovation and shared learning. Support efforts to spur the next generation of vaccination, screening and preventive treatment technologies; programmatic innovations; and scalable approaches; and share new learning broadly.
- Track commitments and encourage accountability. Establish systems to track global progress in expanding coverage, monitor resource investments and compare levels of investment against global commitments and need.
The Initiative partners currently are developing a joint strategy for action focusing on the four goals. News about the Initiative will be posted on the CCA website (www.cervicalcanceraction.org). CCA is functioning as the secretariat for the Initiative for at least the first two years.
Conclusion
Cervical cancer is an eminently preventable disease. We now have the tools in hand to protect girls and women no matter where they live. The global community is coming together to raise awareness of these opportunities, at national and international levels, to mobilize resources to build population-level screening and preventive treatment programmes and to offer vaccination to all young adolescent girls. Of special note is the Initiative launched in London last year and a new collaboration across a variety of United Nations organizations. UN Secretary-General Ban Ki-moon specifically called out the need for progress on cervical cancer prevention in his World Cancer Day statement issued 4 February 2016 (23). Just as we have made tremendous progress during the past decade preventing deaths due to pregnancy-related complications and HIV infection, we now also can save women of all ages from the horrific consequences of cervical cancer.
Resources for further information
- Comprehensive Cervical Cancer Control: A Guide to Essential Practice (World Health Organization) www.who.int/reproductivehealth/publications/cancers/cervical-cancer-guide/en/
- Progress in Cervical Cancer Prevention: The CCA Report Card 2015 (Cervical Cancer Action) www.cervicalcanceraction.org/pubs/CCA_reportcard_low-res_2015.pdf
- RHO Cervical Cancer library (an online resource for information and tools from the leading cervical cancer agencies worldwide, maintained by PATH) www.rho.org
Biographies
Dr Joanna Cain is Professor of Ob/Gyn and Radiation Oncology and Director of Faculty Talent Management, University of Massachusetts School of Medicine. She has practised gynecologic oncology for over 30 years after a fellowship at Sloan Kettering and oversees faculty development. She has been Chair of the subcommittee on Cervical Cancer Control of FIGO and Scientific Programme Chair for FIGO 2015. She serves as Chair of the Advisory Committee for HPV Vaccine Trials for the NCI, as well as continuing her work in women’s cancers globally and expanding models for physician education, development, and advancement in academic medical centres.
Ambassador Sally Cowal is the Senior Vice President for Global Cancer Control at the American Cancer Society. She leads the Society’s efforts to make international cancer control a priority within global health efforts and to amplify proven strategies for prevention, screening, treatment, patient support and pain relief in low- and middle-income countries where the need is greatest. She has been with ACS for the last two years having previously worked at Population Services International, UNAIDS and as a United States diplomat.
Dr David Fleming is PATH’s Vice President of Public Health and oversees programmes in reproductive health, maternal newborn and child health and nutrition, noncommunicable diseases, malaria control and elimination, HIV/AIDS and tuberculosis, health strengthening systems and digital health solutions. He has worked in the past as the Director of the Seattle and King County Health Department, as the Director of Global Health Strategies at the Gates Foundation and as the Deputy Director of the CDC.
Catherine Guinard is Public Affairs Manager at Cancer Research UK, where she advocates on policy issues affecting cancer patients at the European Union and international level. Cancer Research UK is the largest independent funder of cancer research worldwide. The organization plays a key role in the development of new policies across the patient pathway that help beat cancer sooner.
Dr Jose Jeronimo is a gynecologic oncologist who currently serves as Senior Advisor for Women’s Cancers at PATH. He completed his MD degree in Peru, later becoming a staff scientist at the United States’ National Cancer Institute. Since 2008 Jose has implemented operational research projects related to breast and cervical cancer at PATH. He leads the implementation of HPV testing approaches in developing countries and is also the development lead of new treatment options for precancerous lesions of the uterine cervix. Dr Jeronimo is a member of the board of directors of the International Papilloma Virus Society.
Dr Debbie Saslow, PhD, has served as the Director of Breast and Gynecologic Cancer at the American Cancer Society for the past 18 years and is Director, Cancer Control Intervention for HPV Vaccination and Women’s Cancers. She ensures that information and policies related to women’s cancers are scientifically accurate and current, and has been instrumental in building collaborative relationships with organizations across the public, private, and not-for-profit sectors globally as well as within the United States. Dr Saslow is also the Principal Investigator on two cooperative agreements to increase HPV vaccination, and serves as the Vice-Chair of the National HPV Vaccination Roundtable.
References
1. World Health Organization (WHO) International Agency for Research on Cancer (IARC): GLOBOCAN 2012: Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012 [cervical cancer fact sheet]. Available at: http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx.
2. WHO: Health Statistics and Information Systems. Projections of Mortality and causes of death 2015 and 2030. Available at: http://www.who.int/healthinfo/global_burden_disease/projections/en/.
3. Bloom DE, Cafiero ET, Jané-Llopis E, et al. The Global Economic Burden of Non-communicable Diseases. Geneva: World Economic Forum; 2011.
4. Muñoz N, Castellsagué X, de González AB, et al. Chapter 1: HPV in the etiology of human cancer. Vaccine. 2006;24 Suppl 3:S3/1–10.
5. WHO. Comprehensive cervical cancer control: a guide to essential practice. 2nd ed. Geneva: WHO; 2014. Available at: http://apps.who.int/iris/bitstream/10665/144785/1/9789241548953_eng.pdf?ua=1.
6. Schiffman M, Castle PE, Jeronimo J, et al. Human papillomavirus and cervical cancer. Lancet. 2007;370:890–907.
7. de Sanjosé S, Quint WG, Alemany L, et al. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol. 2010;(11):1048–1056.
8. Serrano B, de Sanjosé S, Tous S, et al. Human papillomavirus genotype attribution for HPVs 6, 11, 16, 18, 31, 33, 45, 52 and 58 in female anogenital lesions. Eur J Cancer. 2015;51(13):1732–1741.
9. Stokley S, Jeyarajah J, Yankey D, et al. Human papillomavirus vaccination coverage among adolescents, 2007–2013, and postlicensure vaccine safety monitoring, 2006–2014. United States Morbidity and Mortality Weekly Report. 2014; 63(29);620–624.
10. WHO Global Advisory Committee on Vaccine Safety. Global Advisory Committee on Vaccine Safety Statement on Safety of HPV Vaccines. Geneva: WHO; 2015. Available at: http://www.who.int/vaccine_safety/committee/GACVS_HPV_statement_17Dec2015.pdf?ua=1.
11. Joura EA, Giuliano AR, Iversen O, et al. A 9-valent HPV vaccine against infection and intraepithelial neoplasia in women. N Engl J Med. 2015;372:711–723.
12. Cervical Cancer Action (CCA). Progress in Cervical Cancer Prevention: The CCA Report Card 2015. Seattle: CCA; 2015. Available at: http://www.cervicalcanceraction.org/pubs/CCA_reportcard_low- res_2015.pdf.
13. Sankaranarayanan R, Nene BM, Shastri SS, et al. HPV screening for cervical cancer in rural India. N Engl J Med. 2009;360(14):1385–1394.
14. Tsu V, Jeronimo J. Visual inspection of the cervix: progress to date and the rationale for continued investment. Cancer Control. 2014;84–90. Available at: https://www.cancercontrol.info/articles-from-cancer-care-2014/.
15. Campos NG, Tsu V, Jeronimo J, et al. When and how often to screen for cervical cancer in three low-and middle-income countries: A cost-effectiveness analysis. Papillomavirus Res. 2015;1:38–58.
16. Bansil P, Wittet S, Lim JL, et al. Acceptability of self-collection sampling for HPV-DNA testing in low-resource settings: a mixed methods approach. BMC Public Health. 2014;14:596.
17. Dolman L, Sauvaget C, Muwonge R, et al. Meta-analysis of the efficacy of cold coagulation as a treatment method for cervical intraepithelial neoplasia: a systematic review. BJOG. 2014;121:929–42.
18. WHO. Scaling up action against noncommunicable diseases: How much will it cost? Geneva: WHO; 2011. Available at: http://www.who.int/nmh/publications/cost_of_inaction/en/.
19. Campos NG, Sharma M, Clark A, et al. [unpublished report]. The Cost of Action: A Research Initiative to Determine the Global Price of Comprehensive Global Cervical Cancer Prevention and Control. Boston: Harvard T.H. Chan School of Public Health, Center for Health Decision Science; 2015.
20. CCA. Global Maps. 2015. Available at: http://www.cervicalcanceraction.org/comments/maps.php.
21. CCA. Investing in Cervical Cancer Prevention 2015–2020: Meeting Report, London, November 3 & 4, 2015. Seattle: CCA; 2015. Available at: http://www.cervicalcanceraction.org/pubs/CCA_london_meeting_report_2015.pdf.
22. Page on Taking Cervical Cancer Prevention to Scale: Protecting All Women and Girls. CCA website. Available at: http://www.cervicalcanceraction.org/initiative/index.php. Accessed February 22, 2016.
23. With focus on cervical cancer, Ban says where people live should not determine chances of survival [press release.] Geneva: United Nations News Centre; February 4, 2016. Available at: http://www.un.org/apps/news/story.asp?NewsID=53161#.VsvjX_L2bnE.