Tran Van Thuan, Pham Tuan Anh and Dao Van Tu, National Cancer Hospital, Hanoi, Vietnam and National Institute For Cancer Control, Hanoi, Vietnam, and Tran Thi Thanh Huong, National Institute For Cancer Control, Hanoi and Vietnam Hanoi Medical University, Hanoi, Vietnam
This article looks at the current situation of cancer control is in Vietnam, which is a lower-middle-income country in South East Asia. It highlights the advances that have been made in capacity-building and in spreading knowledge about cancer to improve early diagnosis and treatment. The article also sets out the key challenges that the country still faces including policy development, resources and the need to develop partnerships with other developed regions of the world.
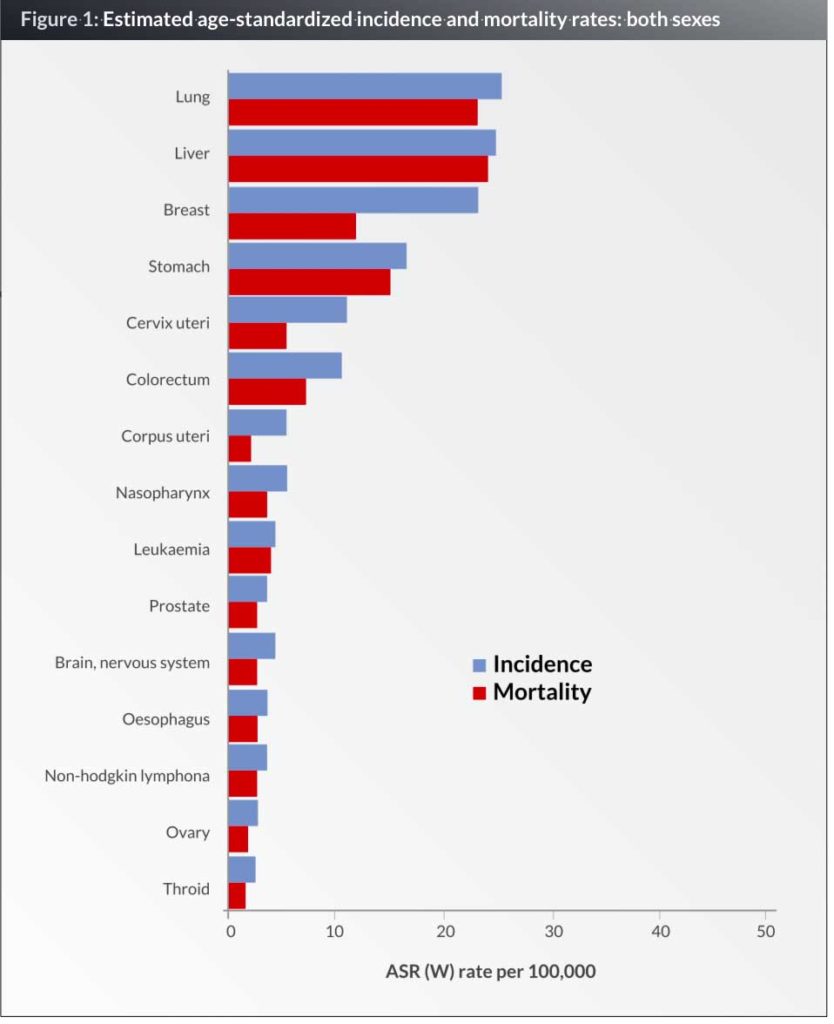
The cancer incidence rates for all cancers per 100,000 persons, which have been reported by the International Agency for Research on Cancer (IACR) in 2012, are 173 for males and 114.3 for females. These incidence rates indicate a national cancer incidence of 125,000 new cases per year for both sexes. IARC estimates cancer mortality rates of 148 per 100,000 for males, 76.3 per 100,000 for females and 94,700 people died from cancer each year. Five year prevalent cases were reported to be 211,800. The top five most frequent cancers in Viet Nam in males and females are cancers of the liver (17.6 % of new cases), lung (17.5 % of new cases), stomach (11.4% of new cases), breast (8.9% of new cases) and colorectum (7 % of all new cases) (1, 2).
The first cancer registry in Viet Nam was established in 1984 in Hanoi. Then, six cancer registries were developed in Ha Noi, Hai Phong, Thai Nguyen, Ho Chi Minh and Can Tho (3). In recent years, three new cancer registries were created. Each cancer registry represented one geographical region in Vietnam. Current statistics are based largely on figures from hospital-based registries preventing a proper assessment of national cancer burden. The quality of cancer registries is variable among the different regions. Nine cancer registries cannot cover the 90 million people in Vietnam. The application of e-hospital records combined with regulations from the Ministry of Health on cancer registry reporting should improve the quality and coverage of cancer registries.
Risk factors and cancer prevention
Life style risk factors
Examination of Figure 1 reveals that there are some key changes that emerge in the pattern of cancer incidence in Viet Nam. We have relatively high rates of lung, gastric, colorectal and breast because of tobacco use, exposure to occupational carcinogens, the ageing of the Vietnamese population and increases in life expectancy, alcohol and obesity due to changing lifestyles.
Lung cancer is also prevented by tobacco control. Viet Nam was successful in introducing a tobacco ban law that was issued by Parliament in 2012 (4). Viet Nam has signed and ratified the WHO Framework Convention on Tobacco Control (FCTC). To date, anti-tobacco actions have included banning direct and indirect advertising of tobacco products, increasing taxation on tobacco products, warning labels on tobacco products, health education in the community and the prohibition of smoking in many indoor environments. The prevalence of tobacco use has declined in males from 56.1% in 2002 to 47.4% in 2010; about 1% per year (5). This is equivalent to world prevalence, and is an excellent result for Viet Nam. There has been an important achievement for women; a survey showed that the prevalence of teenage and adult female use of tobacco has remained below 6% in this decade (5). This means that most tobacco-related cancers in women are most likely to have resulted from passive exposure to male smoking. A major cancer prevention priority in Viet Nam for the coming years is to get adult men to quit smoking.
A national survey on other cancer risk factors showed that among drinking men, 25% were drinking at a hazardous level (≥ 60gr alcohol/day), 80% of people were not eating enough fruit and vegetables, 29% of people were physically inactive, 10.9% of people had obesity, salt consumption/person/day was
10–15 gr (2–3 times higher than what is recommended by WHO) (6).
Infections
Figure 1 also revealed that cancers related to infection account for three of the six most common: liver, gastric and cervical cancers. Liver cancer is often causally associated with infection by the hepatitis B virus (HBV). Most newborn Vietnamese children are now being immunized against HBV. The increased availability and access to the HBV vaccine could offer significant opportunities to reduce liver cancer incidence and mortality in Viet Nam in the coming decades. Cervical cancer is associated with infection by certain types of human papillomavirus (HPV). HPV vaccination is now being piloted. During 2008–2010, a Gavi programme provided HPV vaccination for 6,000 teenagers in some provinces (7). Because of the high cost of vaccination against the HPV16 and 18, it is not a feasible national cancer control strategy at the moment. However, HPV vaccination will be mentioned in the national expanded immunization programme in the next few years.
Environmental factors
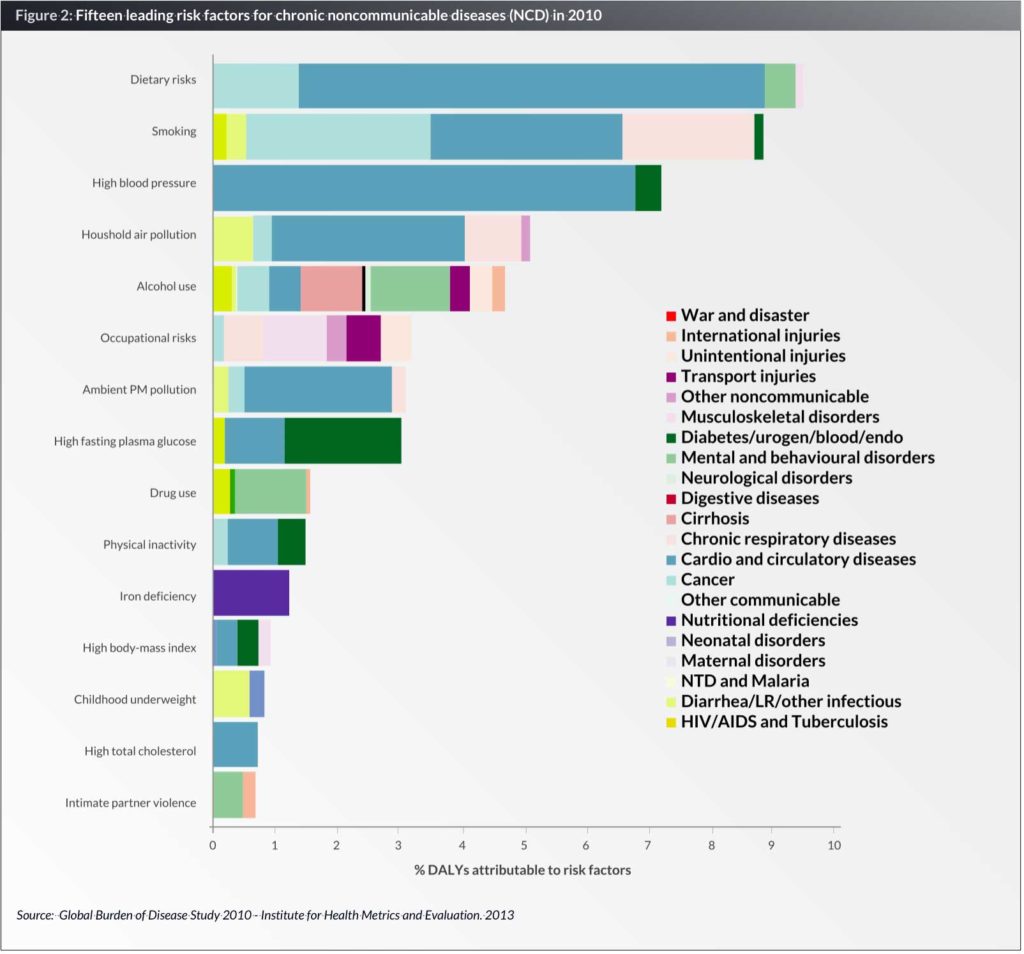
Diet is associated with a reduced or increased risk of cancer. In Viet Nam, diet, smoking and air pollution account for three of the four most common risk factors for chronic noncommunicable diseases in Viet Nam (Fig. 2) (6). Compounds in foods may be carcinogenesis or have anticancer activity. Policies for the control of food safety, hygiene, as well as enironmental pollution, are continuing priorities for the next period.
Hereditary factors
A correlation between hereditary factors and cancer is shown by various studies. In Viet Nam, there are limited research capabilities for cancer molecular biology. The highest quality study is a multicentre one on lung cancer showing 60% of Vietnamese non-small cell lung cancer patients expose the EGFR mutation (8). More study is needed in this field in Viet Nam.
In conclusion, the progress on the primary prevention of cancer in Viet Nam in recent decades has been impressive, but there is still much to be and policies to implement as well as giving cancer education to people and health-care providers about cancer prevention.
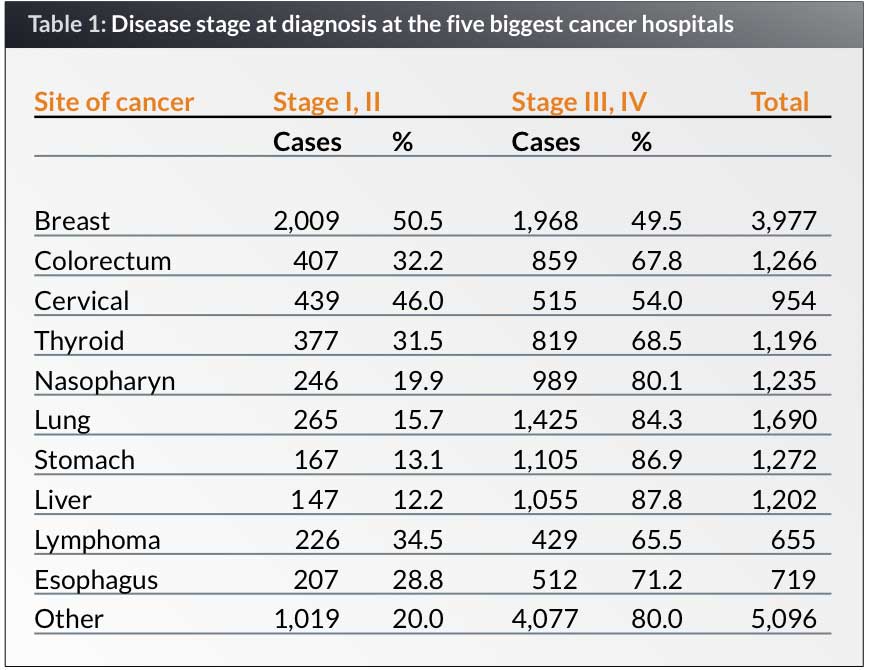
Screening and early detection
Screening and early detection are shown to be effective in curing and improving survival from cancers. In a retrospective study on cancer stages at the five biggest cancer hospitals in Viet Nam in 2009, the results showed that most of cancer patients came and were diagnosed at a late stage. Of newly diagnosed patients, there were respectively 87.8%, 86.9%, 84.3%, 67.8% and 49.5% with liver, stomach, lung, colorectal and breast cancer that presented with stages III and IV at diagnosis (2).
During 2008–2015, a screening programme including cervical, breast, oral and colorectal cancers has been implemented with the support of the National Cancer Control Programme. A 100,000 women aged 30-54 were screened for cervical cancer and breast cancer, 9,634 people were screened for oral and colorectal cancer during 2008–2010 (9). However, breast and cervical cancer screening has been only been implemented in a few populations due to low levels of resource. The limitations of the screening programme is also lacking follow-up. With support from the International Atomic Energy Agency (IAEA), during 2015–2016, 24,000 women in Hanoi and Can Tho were screened for cervical and breast cancer by applying breast cancer examination and VIA techniques. The procedure for following up is also tested. The cancer screening is set up and organized by a health-care team from the central or provincial hospital who come to the community. This is costly and difficult to do annually. Raising awareness of women in the community for regular check ups, improving the knowledge of health-care providers in primary care is also necessary. Choosing the appropriate techniques for screening in a low-middle-income country must be considered.
Knowledge, people’s beliefs on cancer in the community
The results from a study on 20,000 people across 20 provinces/cities in 2010 on their knowledge, beliefs and behaviours of people on cancer prevention showed that only 28.7% of people have a correct knowledge of cancer, and 48.3% of participants thought that surgery will make cancer patients die sooner (10). That is why the aims of national cancer control programme is to increase to 70% people in community have a correct understanding of cancer prevention and that 100% of health-care staff working in provincial and district hospitals are trained on cancer prevention and early detection by 2017.
The majority of patients present with an advanced disease that is not curable. They are mostly from rural Viet Nam, with little access to money and have limited education. The problem of late diagnosis is often due to a variety of factors, but these commonly include a lack of awareness of cancer signs, a lack of money to travel to a hospital and cover the costs of diagnosis and treatment, which thus leads many to seek traditional treatments instead. However, other research shows that even in urban areas there are still a number of barriers to overcome to improve cancer screening. There is a lack of encouragement from health-care system, hence people do not understand the role of cancer screening well enough and cancer screening is not included in health insurance. This research also reveals people’s knowledge on cancer warning signals is still low. The rate of people who knew more than four cancer warning signals was only 22.3%, and 19.7% of interviewees could not name any warning signal at all (10). Therefore, in near future, we will collaborate with the appropriate authorities in establishing a well organized programme of public education to alert people to the early warning symptoms and signs of cancer and encourage those who have any of these warning signs to seek medical advice promptly.
Treatment and diagnosis
One of the significant problems in cancer diagnosis in Viet Nam is the availability of a skilled pathologist in provincial cancer centres. Modern techniques for immune histochemistry and molecular analysis that will drive individual care are also accessible at only a few comprehensive cancer centres. A survey undertaken in 2010 of all 63 provincial hospitals for their capacity for cancer diagnosis and treatment revealed that nine of these 63 hospitals had no functioning pathology departments and that ten could not admit patients with cancer, which meant that they have to refer cancer patients to hospitals with oncology departments (3). Even in specialized cancer centres, accuracy and speed of pathology testing are still challenges that may result in inappropriate treatment and delays in starting treatment.
In radiation, we have the basic techniques of treatment for cancer. We use regular linear machines for external radiation therapy with 3D-conformal radiation therapy techniques. There are 36 machines in whole country. However, in some cancer centres, they still the cobalt-60 external radiotherapy machines because it is not expensive. Intensity-Modulated Radiation Therapy (IMRT) was sparingly used in Viet Nam.
There is limited access to radiotherapy in rural areas. Many provinces do not have access to any radiotherapy treatment facilities as these require financial investment, trained radiotherapy teams, equipment set-up and maintenance, protocols and quality control. For those cancer patients living in provinces without radiotherapy, their only option is to travel to a central cancer centre to access treatment, but few patients from remote areas can afford the considerable expenses involved in treatment in a big city. Surgery and medical oncology are, like all other resources, more likely to be available in urban rather than rural areas.
Many training courses for upgrading knowledge on cancer diagnosis and treatment are regularly organized, but they are lacking on the academic curriculum for oncologists and especially for nurses. Recently, regulations from the Ministry of Health on professional licensing and continuous medical education (CME), gave guidance for specific treatment procedures that can improve the quality of treatment. However, monitoring and quality assurance of the diagnosis and treatment procedures must be developed in the future.
Palliative care
As huge number of cancer patients are diagnosed at the advanced and incurable stage, palliative care for cancer patients in developing countries is critical. More than 70% Vietnamese patients are at the late stage (2). One can imagine that there is a huge need for palliative care and it is an urgent priority as well. However, palliative care for cancer patients is a relatively new cancer specialty in Viet Nam, with the first palliative care department being established in 2000 at the National Cancer Hospital. There are only palliative care units in Ho Chi Minh City and three provincial hospitals. There is no hospice for cancer in Viet Nam. This means that current palliative care services are inadequate for the demand in Viet Nam.
At least 90% of Vietnamese patients die at home in their communes, however palliation of cancer is not provided at commune level (13). Hence developing commune-based palliative care is a high priority. The national cancer hospital has been active in training health-care staff in palliative care. We have conducted many courses for commune health workers and have sent palliative care doctors to work in provincial hospitals to teach palliative care, especially morphine use and psychosocial support.
In the past palliative care patients had limited access to morphine. In 2008, the Ministry of Health issued new guidelines on opiates which means that morphine for pain has been made much more available. Based on revised Opioid Prescribing Regulations, doctors can now prescribe for a maximum of 30 days, instead of seven days, and the dose for a patient is determined by patient need. However, a study on opioid need and usage in 2008 showed that opioid need for patients dying from cancer per year was 126 kg of morphine, but opioid usage was 13.4 kg (about 10%). The authors conclude that oncologists did not prescribe enough morphine (11).
These are the important achievements in palliative care over the last decade, but it remains challenging for next decade. We need government investment and international advocacy in building an effective palliative care network as well as integration of palliative care into the health-care system.
Cost of treatment
The other challenge is to develop evidence-based guidelines adapted for the situation in Viet Nam, a low-middle-income country. The National Cancer Hospital published cancer diagnosis and treatment guidelines for all health-care levels (central, provincial and commune) in 2006. From here, these treatment guidelines have developed and been disseminated, cancer control training courses have been delivered at all levels of the health-care system to strengthen the diagnosis and treatment capabilities. However, more work needs to be carried out for optimal cost-effective cancer treatment. Twinning partnerships with other institutions from developed countries would help us to refine treatment protocols with the best possible therapies within the available resources, provide training programmes with quality curriculum and syllabi to train the next generation of health professionals. We have to merge the international guidelines and our own practices that are appropriate for Vietnamese patients.
In surgical oncology, the price of an operation in Viet Nam is usually cheaper than in other countries in the world. A operation costs from US$ 200 to US$ 1,000 without prosthesis or high-tech equipment (15). We have many surgeons who work in oncology area, however they have not benefited from the same level of education at the surgical hospital or oncology hospital in each region of the country and the quality of surgery depends on the level and specialty of the hospital.
In medical oncology, the price of drugs in Vietnam is high for a lower-middle-income country. In 2011, Viet Nam had the GDP per capita income of US$ 2,052 (13). In Viet Nam, most chemotherapy agents are available, and this provides the principal treatments for cancer patients. Eighty to Hundred percent of chemotherapy is paid by government insurance (14). For all of the early cancers, we can supply the drugs for standard and radical therapy. However, only 30% of new cancer patients are at the early stage. Targeted therapy, molecular therapy and immunotherapy are very expensive and equal to 40–50 times of GDP per capita. There are very few patients, rich patients, who will be able to benenfit from these drugs.
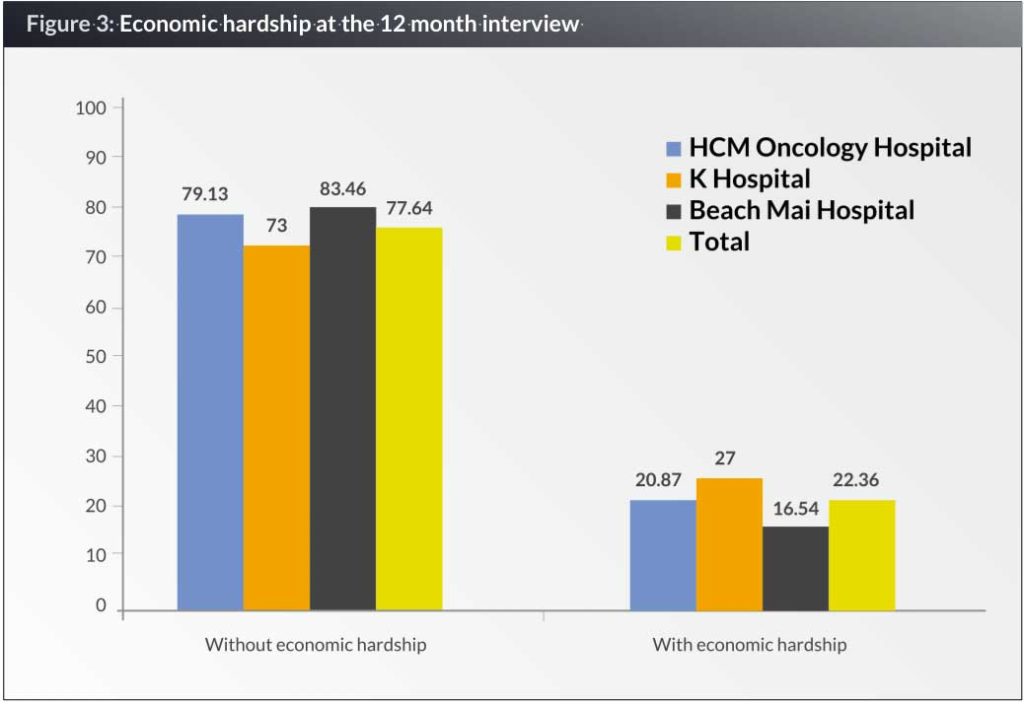
Cancer is an expensive disease to treat and many patients cannot afford to pursue treatment. Health insurance does not cover all treatment fees, especially targeted drugs and high-level technologies. Moreover, patients and their families have to pay for living expenses in big cities such as Hanoi, Ho Chi Minh City that are often expensive. Figure 4 shows 22.36% of cancer patient households (263/1176) suffered economic hardship at a 12 month interview (15).
The lack of affordability of treatment leads to quite high rates of treatment abandonment that result in seeking alternative or traditional treatments or patients not being admitted to hospital for treatment until the cancer is so late that they can only receive palliative care.
National Cancer Network
Infrastructure
Cancer control infrastructure in Viet Nam is still limited although the development of Cancer Control Network over 2011–2020 had been approved by the Ministry of Health. To date there are only three comprehensive cancer centres, and 45 oncology departments in general hospitals in the country. There are shortages of personel, including oncologists and specialized cancer nurses, especially in rural areas. Oncology and palliative care training is often limited in medical schools, which means that doctors and nurses often have to train at the central cancer hospital without an official educational curriculum.
The National Cancer Control Plan (NCCP) was started in 2008 and aims to provide effective diagnosis and treatment. The goals are to build up the cancer workforce and infrastructure with improvements in the quantity and quality of medical staff in cancer control as well as cancer treatment facilities. For example, due to considerable investment, there has been a substantial increase in the number of radiotherapy machines in Viet Nam from 28 teletherapy machines (15 Cobalt and 13 linear accelerators) in 2010 to 36 linear accelerators in 2015. This rapid increase in radiotherapy equipment available to treat patients with cancer has been paralleled by an increase in the number of radiation oncologists, oncology nurses and radiation therapists who operate the radiotherapy equipment. There were approximately 105 radiation oncologists, 49 medical physicists and 98 radiation therapists in 2010. Current data is not available, but there must be huge increase. However these increases in equipment and staff are probably only just keeping up with the increase in the cancer burden, so it is insufficient to meet demand.
Conclusion
In Viet Nam, cancer is a health priority. The National Cancer Control Plan started in 2008. The National Cancer Control Network was approved by the Ministry of Health. The main components of the NCCP are raising awareness of people in the community, the screening and early detection of preventable cancers, improving the knowledge of health-care staff and strengthening monitoring and cancer registry. However, there are still challenges, which include resources, policy development and improving the partnerships for cancer control.
Biographies
Dr Dao Van Tu is a medical oncologist and a research scholar in oncology at the Viet Nam National Institute for Cancer Control and National Cancer Hospital. He obtained his medical degree, residency in medical oncology and clinical fellowship in medical oncology at the Hanoi Medical University, Hanoi, Viet Nam. His research focus on the use of biomarkers in early detection, diagnostics and the treatment of cancer, particularly breast cancer, colorectal cancer and nasopharyngeal cancer. He has also developed an applications using smart phones in both Iphone or Android environments to recruit, communicate and follow-up cancer patients.
Dr Tran Thi Thanh Huong is a medical doctor and psychosocial medicine researcher at Hanoi Medical University, a senior researcher at the National Institute for Cancer Control, and Vice Director of the Bright Future Foundation–Supportive Fund for Cancer Patients. She has extensive expertise in developing, evaluating and capacity building for evidence-based research identifying risk factors for noncommunicable diseases (NCDs), including cancer, mental health, CVD and diabetes. She leads the curriculum development on social determinants of noncommunicable diseases and health psychology for undergraduate and post-graduate students at Hanoi Medical University. Dr Huong is also involved in the development of the National Target Program on Cancer Control in Vietnam and National Network for Cancer Control.
References
1. Fact Sheets by Population [Internet]. [cited 2016 Mar 1]. Available from: http://globocan.iarc.fr/Pages/fact_sheets_population.aspx
2. Bui Dieu, Nguyen ThịHoaiNga, Nguyen Ba Duc, Tran Van Thuan, Le Hoang Minh, Pham Xuan Dung, et al. Cancer Challenges and National Cancer Control Programs to 2020. Viet Nam J. Oncol. 2015;4:13–8.
3. Nguyen Ba Duc et al. Results of national cancer program 2008-2010. Viet Nam J. Oncol. 2010;1:21–6.
4. Government Portal [Internet]. [cited 2016 Mar 1]. Available from: http://www.chinhphu.vn/portal/page/portal/chinhphu/hethongvanban?class_id=1&mode=detail&document_id=163544
5. Global Adult Tobacco Survey (GATS) Viet Nam 2010, Ha Noi, Viet Nam. GATS Viet Nam Working Group;
6. Global Burden of Disease 2010. Institute for Health Metrics and Evaluation; 2013.
7. Tran Van Thuan. Results screening for early detection of cervical cancer in Viet Nam in 2008-2010. Viet Nam Pract. Med. 2011;4:5–7.
8. Shi Y, Au JS-K, Thongprasert S, Srinivasan S, Tsai C-M, Khoa MT, et al. A Prospective, Molecular Epidemiology Study of EGFR Mutations in Asian Patients with Advanced Non–Small-Cell Lung Cancer of Adenocarcinoma Histology (PIONEER). J. Thorac. Oncol. 2014;9:154–62.
9. Tran Van Thuan. National target program on cancer prevention: Results screening for early detection. Viet Nam J. Oncol. 2011;1:15–9.
10. Nguyen Ba Duc et al. Knowledge of cancer early detection in community. Viet Nam J. Oncol. 2011;3-4:43–52.
11. Reyes-Gibby CC. Status of cancer pain in Hanoi, Vietnam: a hospital-wide survey in a tertiary cancer treatment center. J Pain Symptom Manage 2006. 2006;431–9.
12. Vietnam Social Security. Price of drug and health services in Viet Nam 2015. 2015.
13. GDP per capita (current US$) | Data | Table [Internet]. [cited 2016 Mar 2]. Available from: http://data.worldbank.org/indicator/NY.GDP.PCAP.CD
14. Viet Nam Social Security. Law of health insurance [Internet].2008 [cited 2016 Mar 2]. Available from: http://www.baohiemxahoi.gov.vn/Index.aspx?u=doc&su=d&cid=424&id=242
15. The Vietnam National Programme of Action: A decentralization study.